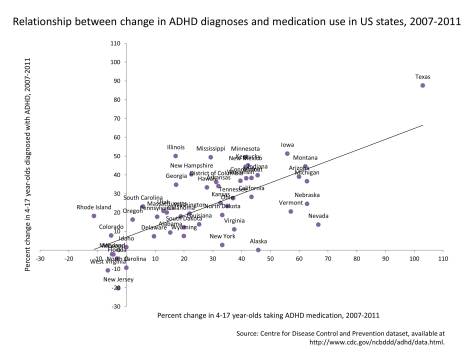
A question closely tied to the issue of prescribing ADHD medication is the actual growth of the disorder. Media reports have cited substantial increases in Ritalin use in the UK, and from looking at prescribing trends in the US one possibility is that the diagnosis of ADHD increases in parallel with growing Ritalin prescriptions. It is particularly important to understand how the increased prescribing of ADHD medication in the UK relates to the actual prevalence of the disorder. However, a key issue in the ADHD debate is whether the diagnosis represents a core developmental disorder. The growth in Ritalin prescriptions and the disproportionately high rates of ADHD in the US in particular have often been used to suggest that ADHD diagnosis is socially motivated.
When we look more closely at the numbers around ADHD, however, three important observations emerge. First, we can see that although there has been a consistent growth in ADHD medication prescriptions in the UK, there is no evidence speaking to whether this also corresponds to an increase in ADHD diagnoses. Second, the common perception of the US being disproportionately affected by ADHD is surprisingly unsupported. Rather, we can see that different methods and approaches to ADHD diagnosis are what best explain its relative prevalence. Third, thinking about ADHD as a label for a highly heterogeneous group can perhaps more readily account for the differential rates of ADHD based on the diagnostic criteria used.
Has the prevalence of ADHD in the UK increased in line with Ritalin prescriptions?
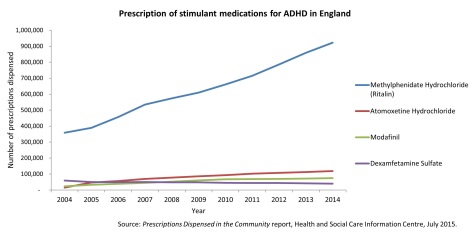
As we saw in our previous blog post, the number of Ritalin prescriptions dispensed in England increased by 156% from 2004 to 2014. However, this does not mean that the prevalence of ADHD has increased by a similar proportion. Why? Factors that can influence the number of prescriptions for ADHD medication written include GPs being more likely to prescribe such medication due to more positive peer-reviewed articles about its effects, changes in prescription protocols (such as more frequent repeat prescriptions being provided), and more awareness amongst parents and the public about the possible benefit of ADHD medication meaning a higher proportion of people ask for medication1. Further, although NICE guidelines published in 2013 recommended treatment for ADHD with medication as part of a comprehensive treatment programme (including psychological, behavioural and educational support), reductions in funding available for such support may contribute to a higher prescription of medication by GPs as an alternative. All of these factors can lead to a higher number of prescriptions being written, and this means the number of prescriptions does not necessarily align with the number of individuals diagnosed with ADHD.
So we need to take a different approach to estimating the prevalence of ADHD diagnoses, by looking at the proportion of actual ADHD diagnoses in the population. However, there are currently no available public health records about ADHD prevalence in the UK. Instead, one useful source of data come from population-based studies, which take a large sample of children (often around 8000-14,000) and estimate the prevalence of ADHD through the percentage of children with parent reports of symptoms and/or ADHD diagnoses. These studies have the benefit of estimating the prevalence of ADHD through a non-referred sample, avoiding the biases arising from estimates reached by only counting the number of children brought to medical attention.
One such study conducted by Green and colleagues in 20042 estimated the UK prevalence of ADHD in 5-15 year-olds at approximately 1.5%. (A similar report from 2003 estimated the prevalence in this age group at 2.2%3). A more recent report by Russell et al. (2014)4 based on the Millenium Cohort Study estimated ADHD prevalence in the UK at 1.4%. This estimate came from data collected in 2008-2009 when children were 6-8 years old, and parents reported whether ADHD had been identified by a doctor or other health professional.
At face value, these figures are a striking contrast to the prescription data: the parent-report data suggest no increase in ADHD diagnoses (from 2004-2009, at least), in contrast to the yearly increase in Ritalin prescriptions over the same time period. However, it is important to consider that the more recent Millennium Cohort Study figures may slightly underestimate the prevalence of children affected by ADHD: this is because the Millennium Cohort sample children were younger, and more children are likely to be diagnosed when they are older.
So whilst it is possible that ADHD diagnoses in the UK have increased, we do not have the data to accurately evaluate this change. As we saw in our previous blog post, data from the US would suggest that growing use of ADHD medication does align with increasing diagnoses, but it is difficult to evaluate this relationship for the UK because we do not have statistics from comparable samples of children at different time points. It is particularly important to verify if the actual number of individuals diagnosed with ADHD has increased to understand whether such a growth in prescriptions stems from more diagnoses, a growing trend to provide medication in lieu of other treatment options, or a combination of the two.
But the current wave of Millennium Cohort Study data were recently collected when children were 11 years old, and using these data researchers can assess if more children in the sample have now been diagnosed with ADHD as they have gotten older – so we might have an answer soon.
Is the United States disproportionately affected by cases of ADHD, and does this tell us anything about causality?
The growth of ADHD medication use and the concurrent prevalence of the disorder is closely related to the debate around whether it reflects an increase in a genuine developmental disorder, or whether such growth is part of a cultural trend towards diagnosis. The geographical vagaries of ADHD in the US particularly have often been invoked as an argument against its legitimacy as a disorder, with some suggestion that the US peak in ADHD rates indicates its diagnosis can be culturally motivated. Sir Ken Robinson, an author, speaker and education adviser, gave a popular TED talk in 2010 in which he showed a map of ADHD prescription rates across the USA, indicating that they increased as one moved east across the country – or as put by Sir Ken, “people start losing interest in Oklahoma, they can hardly think straight in Arkansas, and by the time they get to Washington they’ve lost it completely.”
This brings us to our next question: is it really the case that ADHD is over diagnosed in the US relative to the rest of the world, as media discussion often suggests? The geographical distribution of ADHD is important for two reasons. First, consistent differences in the geographical spread of ADHD may offer clues as to its aetiology: possible environmental causation in areas of high rates, and preventative factors in areas of low rates. Second, the worldwide distribution of ADHD informs the debate on whether it stems from cultural factors which make it an ‘American’ disorder – whatever this may mean – in which case we would expect it to be more prevalent in the US than anywhere else.
When we look at just the US and UK, it appears that US does have higher diagnosis rate of 6.3% (as reported by Russell et al., 2014). This is the closest estimate using the same sampling methods as the UK figure of 1.4% from the Millennium Cohort Study. However, as pointed out in the Millennium Cohort report by Russell et al., there is an explanation for this: a difference in the measurement of ADHD between the US and UK. When the data were collected the DSM-IV was used in the US, but researchers in the UK from whom the data were collected mainly used the ICD-10. The ICD-10 is more stringent, in which a child must show symptoms in all three dimensions of inattention, hyperactivity, and impulsivity to be diagnosed with ADHD, with no comorbid disorders. The DSM-IV is less stringent in the classification of ADHD, whereby children can be diagnosed with symptoms in one dimension only (such as inattention) alongside comorbid disorders. This difference in relative preference of diagnostic criteria can at least partly explain why the DSM-IV-using US has an epidemic compared to the relative calm of the ICD-10-preferring UK5.
When we look at the geographical spread of ADHD across the rest of the world, the figures are particularly striking. A meta-analysis by Polanczyk et al. in 20076 combined 102 studies, comprising data from 171,756 children, to estimate the average prevalence rates reported from samples worldwide in the previous 25 years. This figure was 5.3%. Second, they evaluated whether the US prevalence rates really did exceed everywhere else in the world, relative to Africa, Asia, Europe (excluding the UK), the Middle East, Oceania, and South America. The US rate of 6.2% did not significantly differ from the European rate (4.6%), or the highest rate in South America (11.8%). And importantly, there was no overall association between geographic location and ADHD prevalence rates when the methodology of the studies was controlled for. The figure below shows the prevalence estimates for each region (the bars represent the variability in this estimate).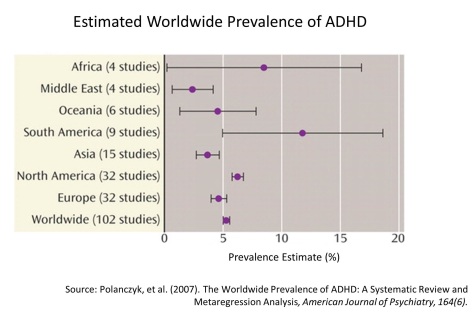
Finally, Polanczyk and colleagues verified that the different ADHD prevalence estimates between the US and Europe in particular were indeed explained by the different diagnostic criteria of the DSM and ICD. They did this by coding for all the methodological features in each study, and found that US diagnoses were more frequently made on DSM criteria, and European diagnoses more so on ICD-10 criteria. Another meta-analysis by Willcutt (2012)7 also found that differences in ADHD prevalence across countries were not significant after diagnostic approaches were controlled for. So these data suggest that ADHD is not disproportionately prevalent in the US; rather, its relative prevalence seems to depend more on the diagnostic tool used.
But on an individual level, any parent of a child with ADHD, or any individual with ADHD, is unlikely to attest that their difficulties with learning, concentration and communication are because they are living in Bolivia rather than Finland. The critical ongoing issue is therefore what constitutes our diagnosis of ADHD. In practice, a child is likely to be identified with ADHD because of how their various cognitive difficulties are expressed, and how this expression is interpreted by clinicians. Part of this interpretation may be due to less quantifiable environmental, social and cultural factors: in particular, Conrad and Bergey (2014)8 recognise that the historical approach to ADHD and medication use in a country can greatly influence whether clinicians classify children’s difficulties under the ADHD diagnostic label. But the different diagnostic criteria of the DSM and ICD do play a role. As noted by Russell et al. (2014), children with hyperactive behaviour and social difficulties may be more likely to be diagnosed with autism spectrum disorder in the UK (due to ICD-10 criteria ruling out a combined diagnosis), and ADHD in the US (due to the DSM-IV allowing ADHD to be diagnosed alongside other developmental disorders). It therefore seems that ADHD is not disproportionately prevalent in the US when we take diagnosis methods into account, but that fact that different tools can yield different prevalence rates makes it important to verify what the ADHD diagnostic label is mapping onto.
A dimensional approach to ADHD
At first glance, quantifying the prevalence of ADHD would suggest counting all children and adults struggling with attention, hyperactivity, and impulsivity and suggesting those individuals reflect the relative rate of ADHD in a particular population. In practise, however, there is no natural threshold between affected and unaffected individuals with ADHD. ADHD can frequently co-occur with other developmental disorders, such as autism spectrum disorder (ASD); in the Millennium Cohort dataset, 24% of the children with ADHD were also diagnosed with ASD. This individual variation supports a dimensional approach to classifying developmental disorders, which considers the extent to which various cognitive difficulties are present rather than a clear-cut diagnostic label.
This is critical in deciding how we give children help in the classroom. For example, we have seen previously that children with poor working memory and children with ADHD have highly similar working memory and executive function deficits, indicating that these shared difficulties are not limited to children with ADHD. Further, although an estimated 25-40% of children with ADHD also have dyslexia9, the treatment approaches for ADHD do not usually address reading difficulties, even though these can be a main constraint on a child’s progress at school. The diagnostic label of ADHD thus represents a highly heterogeneous group of children, and what best helps one child with ADHD may not be what best helps another.
But one might argue that neuroimaging data suggesting reduced prefrontal cortex activity in ADHD is indicative of a clear group of children who suffer from a specific neurobiological disorder. However, even such neurobiological ‘markers’ of ADHD are present to a varying degree in individuals without ADHD. Shaw et al. (2007)10 reported that the age of reaching peak cortical thickness – a measure of brain maturation, before cortical thinning proceeds throughout late childhood and adolescence – was delayed in children with ADHD relative to typically developing children. This finding suggested that ADHD may reflect a delay in typical brain development, rather than a qualitative difference between children with and without an ADHD diagnosis. And Shaw et al. (2011)11 found that this rate of cortical thinning was related to the degree of hyperactive and impulsive symptoms in typically developing children without an ADHD diagnosis. Children with higher ratings of hyperactive/impulsive symptoms had a slower rate of cortical thinning, similar to what was observed in children with ADHD. These data align with the idea that ADHD may be a disorder that is better understood dimensionally, with those who are affected being at the end of a continuum of inattention and/or hyperactivity symptoms, rather than there being a distinct cut-off between ADHD and ‘typical’ development.
How does this inform the question on whether ADHD exists as a developmental disorder? From the evidence above it seems that the label of ADHD does not identify a separate category of children who are inattentive and hyperactive. Rather, what we think of as ADHD is a complex cluster of cognitive and behavioural difficulties which fall on a scale for all children, from unaffected to severe. It is how these difficulties are expressed by children and interpreted by different diagnostic approaches, in different cultural contexts, which determine the cut-off at which a child is diagnosed. Whilst difficult to unpick, these factors may best capture how ADHD is identified and why prescriptions have steadily grown; however, we critically need further data to accurately evaluate ADHD growth in the UK. And on an individual level, the symptoms of ADHD have a substantial impact on the day-to-day lives of those who are affected. It is important we ensure that diagnosis appropriately reflects individual differences between children, and think about how to best to commission education and health services to help affected children and adults.
References
- Prescribing in primary care: Understanding what shapes GPs’ prescribing choices and how might these be changed, RAND Technical Report. Available at http://www.nao.org.uk/wp-content/uploads/2007/05/TR443_3C.pdf
- Green, H., McGinnity, A., Meltzer, H., & Ford, T. G., R. (2004). Mental health of children and young people in Great Britain, 2004. Report commissioned by the Office for National Statistics.
- Reported in the NICE Guidelines pp. 26, available here: https://www.nice.org.uk/guidance/cg72/resources/cg72-attention-deficit-hyperactivity-disorder-adhd-full-guideline-2
- Russell, G., Rodgers, L. R., Ukoumunne, O. C., & Ford, T. (2014). Prevalence of parent-reported ASD and ADHD in the UK: findings from the Millennium Cohort Study. J Autism Dev Disord, 44(1), 31-40. doi: 10.1007/s10803-013-1849-0
- For interested readers, there is also an excellent timeline here depicting ADHD rates in the US as diagnostic tools have changed from 1970 to the present day.
- Polanczyk, G., de Lima, M. S., Horta, B. L., & Biederman. J. (2007). The Worldwide Prevalance of ADHD: A Systematic Review and Metaregression Analysis. American Journal of Psychiatry, 164(6). 942-948.
- Willcutt, E. G. (2012). The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics, 9(3), 490-499. doi: 10.1007/s13311-012-0135-8
- Conrad, P., & Bergey, M. R. (2014). The impending globalization of ADHD: notes on the expansion and growth of a medicalized disorder. Soc Sci Med, 122, 31-43. doi: 10.1016/j.socscimed.2014.10.019
- Reported in Eden, G. F., & Vaidya, C. J. (2008). ADHD and developmental dyslexia: two pathways leading to impaired learning. Ann N Y Acad Sci, 1145, 316-327. doi: 10.1196/annals.1416.022
- Shaw, P., Eckstrand, K., Sharp, W., Blumenthal, J., Lerch, J. P., Greenstein, D., . . . Rapoport, J. L. (2007). Attention-deficit/hyperactivity disorder is characterized by a delay in cortical maturation. Proc Natl Acad Sci U S A, 104(49), 19649-19654. doi: 10.1073/pnas.0707741104
- Shaw, P., Gilliam, M., Liverpool, M., Weddle, C., Malek, M., Sharp, W., . . . Giedd, J. (2011). Cortical development in typically developing children with symptoms of hyperactivity and impulsivity: support for a dimensional view of attention deficit hyperactivity disorder. Am J Psychiatry, 168(2), 143-151. doi: 10.1176/appi.ajp.2010.10030385